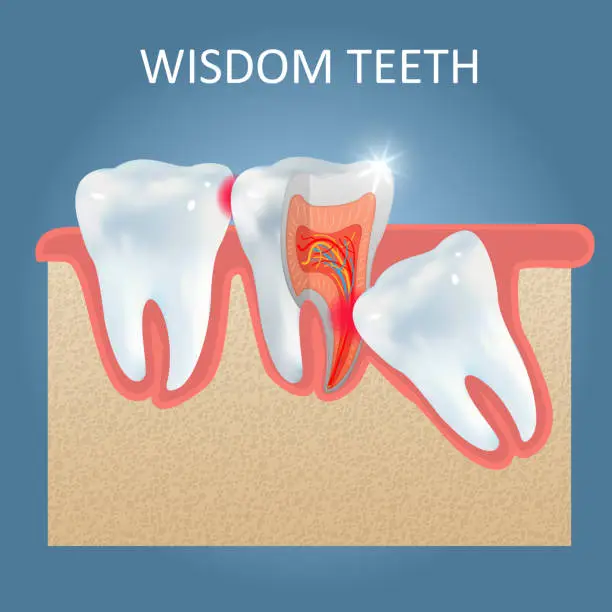
Wisdom Teeth; are the last teeth to erupt and are located at the very back of the mouth. People call them like this because they usually appear between the ages of 17 and 21, when we are supposed to have gained some ‘wisdom’. Why do dentists remove wisdom teeth? Not all jaws are big enough to have a place for these molars to erupt normally. What happens is that the tooth becomes blocked under the gum and becomes stuck or impacted. An impacted wisdom tooth has the possibility of crowding other teeth or creating painful. and often infected, flaps in the gum. Due also to their very back position in the mouth. erupted wisdom teeth are sometimes very difficult to clean. developing decay and gum disease. What Can Happen If I Don’t Remove My Wisdom Teeth? Aside from the cosmetic repercussions mentioned before, overcrowding can prevent the wisdom tooth from having enough room to erupt, thus becoming impacted. An impacted tooth can be very painful and can lead to very serious infection. We recommend that patients remove their wisdom teeth by the time they are young adults to prevent future problems and allow for proper healing. What If I Am Not Experiencing These Problems? Many patients often ask us why we need to remove our wisdom tooth if it hasn’t erupted yet and isn’t causing any pain. In fact. what you have to know is that the roots of the wisdom tooth will continue to grow. making the extraction more difficult and increasing the potential for complication such as late bone healing . The Surgery Our clinic performs wisdom tooth extractions under local anesthesia, or in a hospital under general anesthesia. After surgery it is common to experience a little bit of swelling and discomfort. But really don’t worry about the pain. since we will give you the best combination of medicines in order to make this procedure almost painless. European Dental Center; best dental clinic in Jordan provide this information about Wisdom Teeth.
Occlusion and Joint Disorders (TMJ Disorders) Do you wake up every morning with muscle pain or stiffness in your jaw, neck, head or even shoulders? Have pain when you hear your jaw joint clicking, popping or grating when opening or closing your mouth? Are you have pain in you ear or feeling pressure inside it? Do you have limited movement of the jaw? If yes, you are having one of the most frequent symptoms of people suffering from temporomandibular joint and muscle disorders; Occlusion and Joint Disorders (TMJDs). What is Occlusion and Joint Disorders? TMJDs are a set of clinical conditions characterized by limitation in jaw movement and pain in the jaw joint and surrounding tissues. The cause of Occlusion and Joint Disorders problems in general start from an injury, but for many people, symptoms seem to start without obvious reason. Sometimes discomfort can be occasional will go away with little or no treatment. Even if symptoms persist, most patients still do not need aggressive Types of treatment for (TMJ Disorders) TMJ pain is usually described as a dull ache in the temporomandibular joint and surrounding areas, such as the ears, neck and shoulders. Some people may have no pain, but still experience jaw functionality difficulties. Other symptoms of TMD include the following: Pain or soreness in the jaw that is more prevalent in the morning or late afternoon. Clicking or popping when opening or closing the mouth. Swelling on the side of the face. Sensitive teeth in the absence of dental problems. An earache in the absence of an infection. Difficulty opening and closing the mouth and/or chewing. Upper and lower teeth that do not align properly (malocclusion). Stiffness or “locked” feeling in the jaw when talking, yawning or eating. Jaw pain when chewing, biting or yawning. Recent changes to the bite. Frequently waking up with headaches or experiencing frequent tension headaches. Your particular TMJ treatment should be determined through consultation with a dental professional highly experienced in temporomandibular joint problems. In most cases the treatment would be wearing a (night guard) which is a custom made occlusal splint that covers the lower teeth and the patient should wear it 10 hours a day for two months, if this didn’t work surgery will be the final treatment. European Dental Center; best dental clinic in Jordan provide this information about Occlusion and Joint Disorders.
mouth ulcer (also termed an oral ulcer, or a mucosal ulcer). What is Mouth Ulcer? is an ulcer that occurs on the mucous membrane of the oral cavity. More plainly, a mouth ulcer is a sore or open lesion in the mouth. Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying cause. causes of oral ulceration The two most common causes of oral ulceration are: local trauma (e.g. rubbing from a sharp edge on a filling) and aphthous stomatitis (“canker sores”). a condition characterized by recurrent formation of oral ulcers for largely unknown reasons. Some consider ulcers on the lips or on the skin around the mouth to be included under the general term oral ulceration (e.g. an ulcer left by rupture of a blister caused by herpes labialis, i.e. a cold sore). Mouth ulcers often cause pain and discomfort, and may alter the person’s choice of food while healing occurs (e.g. avoiding acidic or spicy foods and beverages). They may occur singly or multiple ulcers may occur at the same time (a “crop” of ulcers). Once formed, the ulcer may be maintained by inflammation and/or secondary infection. Aphthous stomatitis (also termed recurrent aphthous stomatits, RAS, and commonly called “canker sores”) is a very common cause of oral ulceration. 10-25% of the general population suffer from this non-contagious condition. The appearance of aphthous stomatitis varies as there are 3 types: minor aphthous ulceration. major aphthous ulceration. herpetiform ulceration. Minor aphthous ulceration is the most common type. presenting with 1-6 small (2-4mm diameter), round/oval ulcers with a yellow-grey color and an erythematous (red) “halo”. These ulcers heal with no permanent scarring in about 7–10 days. Ulcers recur at intervals of about 1–4 months. Major aphthous ulceration is less common than the minor type, but produces more severe lesions and symptoms. Major aphthous ulceration presents with larger (>1 cm diameter) ulcers that take much longer to heal (10–40 days) and may leave scarring. The minor and major subtypes of aphthous stomatitis usually produce lesions on the non-keratonized oral mucosa (i.e. the inside of the cheeks, lips, underneath the tongue and the floor of mouth), but less commonly major aphthous ulcers may occur in other parts of the mouth on keratinized mucosal surfaces. The least common type is herpetiform ulceration, so named because the condition resembles primary herpetic gingivostomatitis. The exact cause of aphthous stomatitis is unknown, but there may be a genetic predisposition in some people. Other possible causes include: hematinic deficiency (folate, vitamin B, iron). stopping smoking, stress, menstruation. trauma. food allergies or hypersensitivity to sodium lauryl sulphate (found in many brands of toothpaste). Aphthous stomatitis has no clinically detectable signs or symptoms outside the mouth, but the recurrent ulceration can cause much discomfort to sufferers. The Treatment is aimed at reducing the pain and swelling and speeding healing, and may involve systemic or topical steroids, analgesics (pain killers), antiseptics, anti-inflammatories or barrier pastes to protect the raw area. treatment of Mouth Ulcer Treatment is cause related, but also symptomatic if the underlying cause is unknown or not correctable. It is also important to note that most ulcers will heal completely without any intervention. Treatment can range from simply smoothing or removing a local cause of trauma, to addressing underlying factors such as dry mouth or substituting a problem medication. Maintaining good oral hygiene and use of an antiseptic mouthwashes/sprays (e.g. chlorhexidine) can prevent secondary infection and therefore hasten healing. A topical analgesic (e.g. benzydamine mouthwash) may reduce pain. Topical (gels, creams or inhalers) or systemic steroids may be used to reduce inflammation. An antifungal drug may be used to prevent oral candidiasis developing in those who use prolonged steroids. People with mouth ulcers may prefer to avoid hot or spicy foods, which can increase the pain. Self-inflicted ulceration can be difficult to manage, and psychiatric input may be required in some people. European Dental Center; best dental clinic in Jordan provide this information about Mouth Ulcer.
Oral cancer; is a subtype of head and neck cancer, is any cancerous tissue growth located in the oral cavity. It may arise as a primary lesion originating in any of the oral tissues, by metastasis from a distant site of origin, or by extension from a neighboring anatomic structure, such as the nasal cavity. Alternatively, the oral cancers may originate in any of the tissues of the mouth, and may be of varied histologic types: teratoma. adenocarcinoma derived from a major or minor salivary gland. lymphoma from tonsillar or other lymphoid tissue. melanoma from the pigment-producing cells of the oral mucosa. There are several types of oral cancers, but around 90% are squamous cell carcinomas, originating in the tissues that line the mouth and lips. Oral or mouth cancer most commonly involves the tongue. It may also occur on the floor of the mouth, cheek lining, gingiva (gums), lips, or palate (roof of the mouth). Pathologists typically classify most oral cancers as squamous cell carcinoma because they look very similar under the microscope. Signs and symptoms for Oral cancer Skin lesion, lump, or ulcer that do not resolve in 14 days located: On the tongue, lip, or other mouth areas. Usually small. Most often pale colored, be dark or discolored. Early sign may be a white patch (leukoplakia) or a red patch (erythroplakia) on the soft tissues of the mouth. Usually painless initially. May develop a burning sensation or pain when the tumor is advanced. Behind the wisdom tooth. Even behind the ear. Additional symptoms that may be associated with this disease: Tongue problems. Swallowing difficulty. Mouth sores. Pain and paranesthesia are late symptoms. Tobacco and cancer Smoking and other tobacco use are associated with about 75 percent of oral cancer cases, caused by irritation of the mucous membranes of the mouth from smoke and heat of cigarettes, cigars, and pipes. Tobacco contains over 60 known carcinogens, and the combustion of it, and by products from this process, is the primary mode of involvement. Use of chewing tobacco or snuff causes irritation from direct contact with the mucous membranes. Tobacco use in any form by itself, and even more so in combination with heavy alcohol consumption, continues to be an important risk factor for mouth cancer. However, due to the current trends in the spread of HPV16. Alcohol and Oral cancer The use of alcohol and other toxic liquids is another high-risk activity associated with oral cancer. A very strong synergistic effect on oral cancer risk is known when a person is both a heavy smoker and drinker. The risk greatly increases compared to a heavy smoker or a heavy drinker alone. Alcohol-containing mouthwashes are also considered etiologic agents in the cancer risk family. European Dental Center; best dental clinic in Jordan provide this information about Oral Cancer.
Tooth sensitivity; is tooth discomfort in one or more teeth that is triggered by: hot, cold, sweet, or sour foods and drinks, or even by breathing cold air. The pain can be sharp, sudden, and shoot deep into the nerve endings of your teeth. Sensitive teeth occur when the underlying layer of your teeth –the dentin– becomes exposed as a result of receding gum tissue (the protective blanket that covers the tooth roots). The roots, which are not covered by hard enamel, contain thousands of tiny tubules leading to the tooth’s nerve center (the pulp). These dentinal tubules (or channels) allow the stimuli — for example, the hot, cold, or sweet food — to reach the nerve in your tooth, which results in the pain you feel. What Causes Tooth sensitivity? There are many factors that may lead to sensitive teeth, including: Brushing too hard. Over time, brushing too hard or using a hard-bristled toothbrush can wear down enamel and cause the dentin to be exposed. It can also cause recession of the gums (the gum tissue pulls away from the teeth). Tooth decay near the gum line. Recession of the gums. As gums move away from a tooth due to conditions such as periodontal disease, the root surface becomes exposed. Gum disease (gingivitis). Inflamed and sore gum tissue may cause sensitivity due to the loss of supporting ligaments, which exposes the root surface that leads directly to the nerve of the tooth. Cracked teeth. Chipped or broken teeth may fill with bacteria from plaque and enter the pulp causing Inflammation. Teeth grinding. Grinding or clenching your teeth may wear down the enamel and expose underlying dentin. Tooth whitening products. These products may be major contributors to sensitive teeth. Your age. Tooth sensitivity is highest between the ages of 25 and 30. Plaque build-up. The presence of plaque on the root surfaces can cause sensitivity. Mouthwash use. Long-term use of some mouthwashes. Some over-the-counter mouthwashes contain acids that can worsen tooth sensitivity if you have exposed dentin (the middle layer of the tooth). The acids further damage the dentin layer of the tooth. If you have dentin sensitivity, ask your dentist about the use of a neutral fluoride solution. Acidic foods. Regular consumption of foods with a high acid content, such as citrus fruits, tomatoes, pickles, and tea, can cause enamel erosion. Recent routine dental procedures. Sensitivity can occur following teeth cleaning, root planning, crown placement, and tooth restoration. Sensitivity caused by dental procedures is temporary, usually disappearing in four to six weeks. What Can I Do to Reduce Sensitive teeth? Some steps you can take to prevent tooth sensitivity include: Maintain good oral hygiene. Continue to follow proper brushing and flossing techniques to thoroughly clean all parts of your teeth and mouth. Use a soft bristled toothbrush. This will result in less toothbrush abrasion to the tooth surface and less irritation to your gums. Brush gently and carefully around the gum line so you do not remove more gum tissue. Use desensitizing toothpaste. There are several brands of toothpaste available for sensitive teeth. With regular use you should notice a decrease in sensitivity. You may need to try several different brands to find the product that works best for you. Another tip. spread a thin layer of the toothpaste on the exposed tooth roots with your finger or a Q-tip before you go to bed. Do not use a tartar control toothpaste; rather, use a fluoridated toothpaste. Watch what you eat. Frequent consumption of highly acid foods can gradually dissolve tooth enamel and lead to dentin exposure. They may also aggravate the sensitivity and start the pain reaction. Use fluoridated dental products. Daily use of a fluoridated mouth rinse can decrease sensitivity. Ask your dentist about available products for home use. Avoid teeth grinding. If you grind or clench your teeth, use a mouth guard at night. See your dentist at regular intervals. Get professional tooth cleaning, oral hygiene instructions, and fluoride treatments every six months (or sooner depending Tooth sensitivity on your condition). European Dental Center; best dental clinic in Jordan provide this information about Tooth sensitivity.
Dental sealants are plastic coatings that are commonly placed in the fully erupted permanent molars of children or young adults. They have demonstrated to prevent tooth decay and stop decay if it has not reached the dentin. Sealants are liquid coatings that harden on to the chewing surfaces of teeth and are designed to prevent the intrusion of bacteria. and other debris into the deep crevices on the tops of teeth. The pits and grooves of your teeth are prime areas for opportunistic decay. Even regular brushing sometimes misses these intricate structures on the chewing surfaces of your teeth. Application For Dental Sealants First, the dentist cleans the tooth surface before applying sealants. Then, they etch the tooth with a chemical substance, which enhances the adherence of the sealant. Finally, they direct a light source to the site to harden the material after applying the sealant. When are dental sealants indicated? Sealants are recommended in molars and premolars of children and adults with high susceptibility to dental decay. For example: Molars with deep grooves in patients that do not brush properly or that do not maintain a proper oral hygiene. Patients with several cavities in primary teeth or baby teeth. This is a good indicator of dental decay in permanent teeth. Patients that are motor impaired that have difficulty keeping their teeth free of dental plaque. Dental Health and Fluoride Treatment Fluoride is a mineral that occurs naturally in many foods and water. Acids, formed from plaque bacteria and sugars in the mouth, attack the enamel layer of a tooth, causing demineralization, which results in the loss of minerals. such as: fluoride. calcium. phosphate. Minerals redeposited (remineralization) to the enamel layer from the foods and waters consumed. Fluoride helps prevent tooth decay by making the tooth more resistant to acid attacks from plaque bacteria. and sugars in the mouth. It also reverses early decay. also helps speed remineralization as well as disrupts acid production in already erupted teeth of both children and adults. Salt and city water, toothpastes, and mouth rinses contain fluoride, but dentists can also apply it. People with certain conditions, such as, are specially recommended fluoride application: dry mouth. gum disease. history of frequent cavities and presence of crowns and bridges or braces. “Prevention is cheaper and better that Treatment”. Therefore, we encourage patients to come for regular visits and accept preventive treatments such as sealants and fluoride. Young children are great candidates for preventative measures like sealants and fluoride because in many cases. decay has not set in yet. European Dental Center; best dental clinic in Jordan provide this information about Dental Sealants and Fluoride.
Dentist offer Smoking Cessation; We are sure that you are already aware about the side effects of Cigarette smoking on your body such as lung cancer, stroke, heart attack and even death But did you know that but cigarette smoking takes a enormous toll on your oral Health. oral health consequences oral health consequences we see in patients who smoke: Bad breath. Tooth discoloration. Increased tooth and bone loss. Increased risk of periodontal disease. Lower success rate of dental implants. Delayed healing processes. Why does a Dentist offer Smoking Cessation? Smoking can interfere with the success of dental procedures you have done in our office as well as limit the options we are able to provide you. Smoking has a direct effect on gum and implant healing, reduce surgical prognosis and is responsible for oral cancers. In order to give you the . best results, we will do our best to assist you in smoking cessation Don’t Give up !!! Studies have shown nicotine to be more addictive than heroin, so its safe to say quitting will be one of the most difficult times in your life, but is well worth it! The good news is no matter how many times someone’s tried to quit before, this time could be different. European Dental Center; best dental clinic in Jordan provide this information about Dentist offer Smoking Cessation.
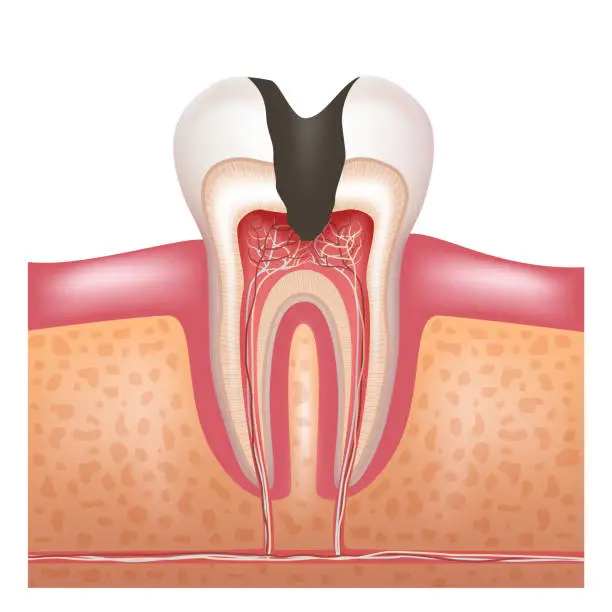
Prevention of dental caries and your tooth from pain is important and easier than dental treatment whatever little cost or facilitates its ways. prevention from dental caries So it is important to follow these instructions for prevention of dental caries: decrease of sweets Eating too much sweets, sugar, tea, and coffee with sugar, soft drinks, and chocolate leads to increased dental caries because all of these contain large amounts of sugar, so you must decrease the administration of food contains the sugar and pay attention for your children do not eat sweets to protect their teeth. Brushing at least twice daily You must brush your teeth immediately after eating of sweets and for your children it’s better to start brushing at time of deciduous teeth eruption, learn and follow them for brushing their teeth Using dental floss It’s better to us dental floss for cleaning among your teeth. Fluoride material Fluoride is important for prevention from dental caries, so adding it to water or putting directly on teeth can protect your teeth. There fore advice giving to dental centers to put fluoride on children teeth twice a year, but attention must be give to avoid taking fluoride more than required limit –This is found in the south Jordan water – and may lead to fluorosis (Stains ranging from yellow to dark brown) also taking large amount of fluoride leading to toxicity, so it mists be away from children. Avoid bottle feeding Continuous bottle feeding lead to cover baby teeth with layers and this lead to early tooth caries, so It’s preferable to avoid taking bottle feeding to your children but if it is got, the mother should clean her baby teeth after each feeding with moisture clean cloth. European Dental Center; best dental clinic in Jordan provide this information about Advises for prevention of dental caries.